When we bill for any payment it’s very easy for us to calculate and pay bills. But when it comes to medical billing like physical therapy services then this process is not as simple as we think. For the right reimbursement, it is important to have the right documentation that must comply with the latest billing regulations. Accurate coding saves practices from denials and compliance issues and ensures on-time payment. One major component of physical therapy billing is an 8-minute rule that helps your practice to know how time-based procedures are billed under Medicare and other insurance plans. To separate the services accurately it is important to have knowledge of Common Procedural Terminology (CPT) codes. All these elements contribute to an efficient billing process. Let’s understand the whole process in detail to know how physical therapists can optimize revenue and maintain compliance.
What is the 8-minute Rule?
In 1998, the Centers for Medicare & Medicaid Services (CMS) introduced a billing standard for physical therapy and other outpatient therapy sessions which is called the 8-minute rule. If you’re seeing Medicare patients, this rule is non-negotiable. And even if you’re dealing with private insurers, many follow the same standard. The purpose of this rule was to calculate the billable units of time-based services accurately. It aligns the reimbursement with the actual time that healthcare providers spend on patient care. The more time you spend, the more units you can bill.
Medicare adds all the minutes of skilled, one-on-one therapy and divides their sum by 15. If providers spent more than 8 minutes then units are counted but when seven or fewer minutes are left then no additional units count. With the help of this rule, therapists accurately bill for the time that they spend on treatment and save practices from overbilling or underbilling. Providers get fairly compensated and ensure compliance with Medicare and insurance regulations.
How the 8-Minute Rule Works
Let’s say you’re providing manual therapy to a patient. If you spend between 8 and 22 minutes on that service then you can bill one unit of manual therapy with CPT code 97140. If you go beyond 22 minutes then you can bill two units. The rule applies in chunks of 15 minutes but you can only bill a unit when you spent at least an 8-minute threshold. This time circle includes:
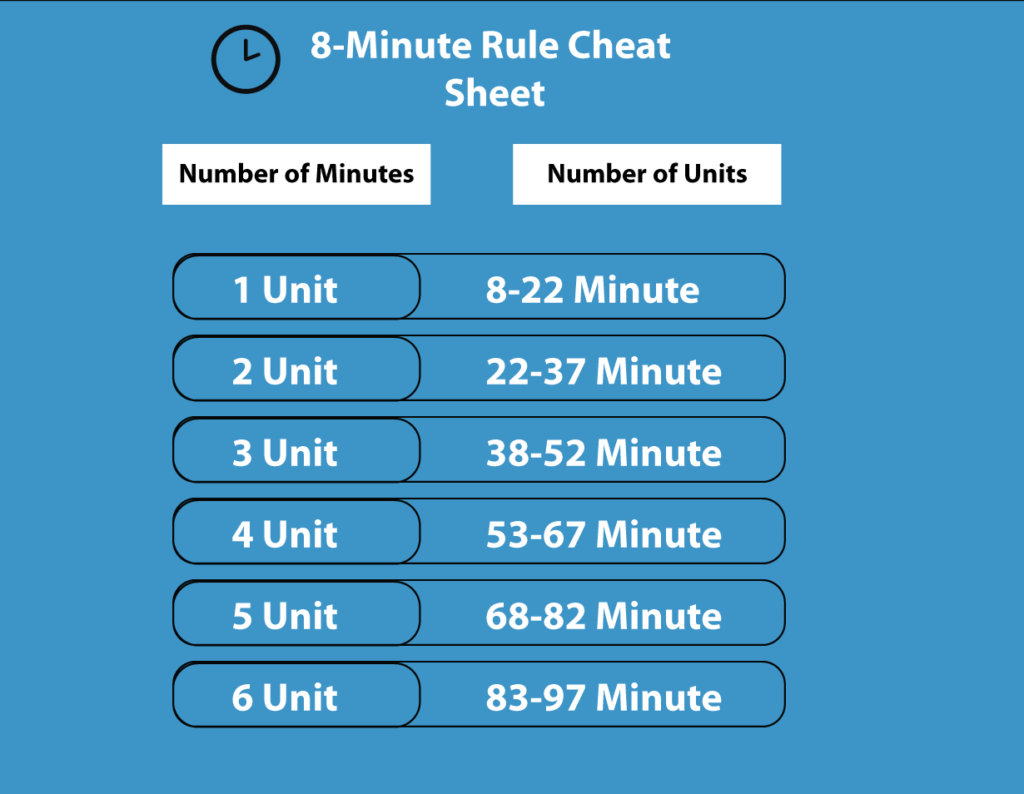
Now, let’s say you provide multiple time-based services in a single session—maybe you do 10 minutes of manual therapy, 12 minutes of therapeutic exercise, and 7 minutes of neuromuscular re-education. If you added up all the minutes, you’d have 29 total minutes of billable time. Since each of these falls below 8 minutes individually, you might wonder how to bill. The trick here is to combine them and apply the rule to the total by giving one unit to the service with the most time and the second unit to the next highest. If you have done 29 minutes then it fits within the 23-37-minute range now you can bill two units total.
Remember that there are some times that healthcare providers spend on patients but it’s not billable. This non-billable time includes:
- Documentation even if done in front of the patient
- Rest periods
- Time spent preparing equipment
- Supervised exercises where you’re not actively engaging the patient
CPT Codes for the 8-Minute Rule
Now that we’ve got the 8-minute rule therapy down, let’s talk about the most commonly used CPT codes in physical therapy.
There are two types of treatment code units that calculate for billing. One is time-based units and the other one is service-based units. Service-based codes are used for services like physical therapy evaluations, hot/cold packs, and group therapy. It is not based on time spent on treating a patient and only one unit is used to bill for these services. There are different physical therapy procedure codes used for service-based treatments including:
- 97001 – Physical therapy evaluation (replaced by 97161-97163)
- 97002 – Physical therapy re-evaluation (replaced by 97164)
- 97014 – Electrical stimulation (unattended)
- G0283 – Electrical stimulation (Medicare-specific)
- 97150 – Group Therapy
- 97010 – Hot or Cold Packs
Now if we talk about the time-based codes then they are based on time like therapeutic exercises, and manual therapy. Healthcare providers must spend at least 8 minutes on time-based services to get reimbursement for each unit. The number of units that can be billed increases based on the total time spent. Both of these codes seem simple but practices face difficulty when they bill both time-based and service-based codes for visits of a single patient. There are different physical therapy CPT codes for time-based services including:
Evaluation Codes
- 97161, 97162, 97163 (Physical Therapy Evaluations)
- 97164 (Re-evaluation)
Therapeutic Procedures (Time-Based)
- 97110 – Therapeutic exercises
- 97112 – Neuromuscular re-education
- 97116 – Gait training
- 97530 – Therapeutic activities
- 97033 – Iontophoresis
- 97535 – Self-care/home management training
Manual Therapy & Modalities
- 97140 – Manual therapy
- 97035 – Ultrasound therapy
- 97032 – Electrical stimulation (manual)
- 97010 – Hot/cold packs (Untimed)
Billing Strategies for Maximum Reimbursement
Proper Documentation Practices
Proper documentation is needed for reimbursement and avoiding claim denials. Proper documentation helps healthcare practices to clearly define medical necessities for each service and record the exact time that they spent on each process. In this documentation, CPT codes are properly linked to relevant diagnosis codes for proper claim submission and describe the whole treatment process.
Avoiding Claim Denials and Audits
Claim denials mostly occur when there’s an error in coding like incorrect CPT coding like using an untimed code when a timed code is right. When healthcare providers lack proper documentation and they fail to justify their services then they can face claim denials. Another reason is missing or using incorrect modifiers like GP modifiers for therapy services under Medicare. When practices face claim denials they pay additional costs that also affect their revenue cycle management system. That’s why healthcare providers need to save their practices from denials by double-checking CPT codes before claim submission. Using modifiers where required like 59 modifiers for different procedural services. They also need to stay updated with insurance policies for compliance.
Using the 8-Minute Rule Efficiently
To add more efficiency to their billing processes therapists can use combined services strategically. For example, if a patient requires both therapeutic exercises CPT code (97110) and neuromuscular re-education (97112) then their time can be split effectively to make sure that both services are properly billed. Try to avoid underutilization because when you utilize available treatment time completely then it benefits both patient and practice revenue. Keep your staff trained on efficient documentation to make sure that no time goes unaccounted for in billing records.
Outsource your Billing Services
Billing for physical therapy gets sometimes frustrating as healthcare providers do not have time to solve the billing issues. The best solution to make their billing processes more efficient and reliable is to outsource billing operations to an experienced medical billing company. These companies have years of experience and they know how to handle these complexities and smooth your revenue cycle management. If you want the best billing services providers then you can choose M&M Claims Care which is an experienced medical billing company that has provided physical therapy billing services for years. They work for your cash flow and help you to achieve your financial goals. M&M Claims Care follows best practices to reduce your practices denied claims and ensure you’re getting paid for the valuable work you do.







